This section of the website was last updated February 17, 2026. We invite you to check back regularly.
-
General Questions
-
Billing System
-
Forming a Blended Capitation Group
-
Incentives, Grants and Stipends
-
Learners
-
Leave
-
Locums
-
Income Floor and Top-Up Payments
-
Capitation Payments
-
Non-Rostered Patients and the FFS Billing Limit (“Cap”)
-
Performance Indicators
-
Practice Facilitation Services
-
Rostering
-
Service Expectations
General Questions
The agreement is appended as Schedule R of the Memorandum of Agreement (MOA) and is available in its entirety here. The latest version is dated September 2, 2025.
Family physicians, who are interested in participating in the Blended Capitation program, must submit an expression of interest form. Please note the form is an expression of interest only and represents an ongoing process—there is no deadline for submission.
To submit your expression of interest, please click here.
- The acceptance date into the Blended Capitation Program is the date the signed Letter Agreement for each physician in your group are received by FPRP. When Blended Capitation Groups (BCGs) are issued letter agreements for review and execution, they have six months for at least three physicians within group to submit their signed letter agreements to FPRP. After six months the letter agreements will be void.
- All of the initial members of your group will have the same acceptance date. Please note that your acceptance date may not be the date that you signed your individual physician’s letter agreement.
- Grants and stipends will be authorized for payment once all physicians within a BCG submit their signed letter agreements.
Participation in the Blended Capitation Model (BCM) is voluntary. Physicians enrolled in the model may voluntarily choose to go back to fee-for-service. Physicians may discontinue their enrolment by submitting a Blended Capitation Withdrawal Form at least 30 days before their desired end date. Upon discontinuance from BCM, the physician shall notify attached patients that the physician will no longer be providing services under the Model.
Once a physician withdraws from BCM their patients will be de-rostered from the BCM billing system and the physician will return to billing 100% FFS. If they wish to rejoin the BCM they will need to re-apply by submitting a new Expression of Interest Form.
As per Section 9 of the BCM Policy Guide, if a physician’s departure reduces their Blended Capitation Group (BCG) to fewer than three physicians, the BCG is expected to make a diligent effort to find a new physician to join the group as quickly as possible. FPRP will monitor the group’s efforts every 12 months and will assist the BCG to identify and connect with other potential group members.
Once a Blended Capitation Withdrawal Form is received by the Family Practice Renewal Program (FPRP), the withdrawing physician will be contacted within 30 days with instructions concerning the return of any owing amounts for pro-rated grants and stipends.
- One-Time Start-Up Grant ($10,000) – pro-rated
- Annual Quality of Care Stipend ($7,500) – pro-rated
- Transition Incentive ($11,250) – not pro-rated
- EMR Transition Grant ($30,000) – not pro-rated
Returning Overpaid One-Time Start-Up Grant and Annual Quality of Care Stipend
The One-Time Start-Up Grant ($10,000) and Annual Quality of Care Stipend ($7,500) are based on one-year participation in the BCM, starting with the acceptance date (i.e., the date upon which the physician’s signed Letter Agreement and initialed Appendices A and B are received by FPRP), and will be pro-rated in the event of a physician’s departure from the Model. Overpaid funds will be recovered from the physician.
Overpayment recoveries will be coordinated by the FPRP and the departing physician will be invoiced for any overpayment with full payment due in 30 days.
The formula for calculating the amount of funds to return is as follows:
- (Full fund amount / 365) x days enrolled in BCM = amount physician retains
- Full fund amount – amount physician retains = amount physician returns
| Example:
Physician enrolled for 90 days and decides to withdraw and return overpaid portion of $10,000 One-Time Start-Up Grant. ($10,000/365 days) x 90 days = $2,465.75 $10,000 – $2,465.75 = $7,534.25 |
Transition Incentive
The Transition Incentive ($11,250) is not pro-rated. Providing a physician has made a full transition to the BCM, no funds will be recovered. However, if a physician withdraws from the Model and later wishes to rejoin, a second Transition Incentive will not be paid.
EMR Transition Grant
The EMR Transition Grant ($30,000) is not pro-rated. Providing a practice has fully transitioned to the Provincial EMR, or is committed to completing the transition process, no funds will be recovered. However, if a practice leaves the Model and later wishes to rejoin, a second EMR Transition Grant will not be available.
Full transition to the Blended Capitation Model
Full transition to the BCM represents 18 months in the model (starting with the physician’s date of acceptance).
Participation in the EMR program does not come with cyber security insurance or advice. CMPA will cover the cost of notifying patients of a breach but no other costs related to a privacy or security breach. The NLMA recommends physicians get cyber security insurance through their own insurers. The Association also recommends physicians, and their staff, complete the cyber security training, eCE Shield offered by eHealth Centre of Excellence. https://ehealthce.ca/Shield.htm.
The one-time start-up grant of $10,000 paid by FPRP to each physician upon acceptance into the Program, and who is part of the blended capitation group at the time of the Group’s establishment, is intended to cover expenses such as those you describe, as well as expenses such as technology, renovations, and professional services. Schedule R does not provide for any additional compensation.
Billing System
FPRP has received no information about any changes to the EMR system or whether/when it would be integrated with EPIC.
A BCG will only begin billing in the new BCM system after it has been onboarded with eDOCSNL support, which will include demos and training. Physicians will continue to bill 100% FFS until they meet with eDOCSNL to be onboarded to the BCM billing system.
When a date for onboarding is suggested by eDOCSNL, BCGs are required to schedule their onboarding within a reasonable timeline from that date (i.e., within 3 months). When you have confirmed your onboarding date with eDOCSNL, please make every reasonable effort to adhere to the date selected unless extenuating circumstances arise. eDOCSNL must allocate dedicated resources to support onboarding blended capitation groups which must be coordinated between supporting other blended cap groups and the many other expectations that eDOCSNL personnel are required to meet. In the event of extenuating circumstances, please communicate with the eDOCSNL team to identify an alternate date.
In preparation for onboarding, accepted blended capitation groups are encouraged to begin enrolling patients as soon as reasonably possible, at a pace that suits their practice. Then, once your blended capitation group is onboarded to the billing system, you can roster all enrolled patients on the first day.
Please note, patients must be enrolled before they can be rostered (attachment is a requirement of Schedule R).
MCP will send a message notifying you that your patient has been de-rostered from their system, which will stop the capitation payment associated with that individual, but the “Blended Capitation” box will remain checked in your EMR billing window. For patients who will be permanently de-rostered, you will need to uncheck the “Blended Capitation” box to ensure patients’ roster status is accurate on your end, so that you are billing appropriately.
The covering physician working in a separate EMR will have to establish that the patient is rostered to a physician in the BC group. They can do this by:
- Asking and taking the word of the patient
- Having access (e.g., view only access) to the other physician’s EMR and verifying (recommended)
They would then indicate in the billing window that the patient is rostered (by checking the Blended Capitation flag on top of the billing window) and then all the bills will subsequently be reduced to 25%.
The above guidance is generalized and BCGs are advised to develop a solution that works for them. An EMR Practice Advisor will help BCGs understand the pros and cons of the potential solutions so they can make an educated decision on workflow for this.
For more information about separate vs single/combined EMR instances, please view this graphic developed by eDOCSNL:
Considerations for joining a common instance or maintaining separate EMRs
Forming a Blended Capitation Group
You can have success with any size group. The size of the BCG impacts many aspects of a practice: physician schedules related to regular, reasonable hours; how competing demands outside of the practice are managed; distribution of after hours responsibilities to name a few considerations. Other provinces have demonstrated success with BCGs of varying sizes.
A group of physicians in the Blended Capitation Model do not need to co-locate in the same physical space. After-hours care for patients within the group can be provided virtually and in-person.
FPRP has a Practice Facilitator who can assist you in finding other physicians who are interested in forming a Blended Capitation Group.
Co-location is not a requirement; groups do not have to be under the same roof.
A Group must consist of at least 3 physicians. Consistent with Schedule R, when a Group falls below 3 Physicians, the goal of the Group and the FPRC is to re-establish the minimum number of Physicians in a reasonable period. It is expected that the Group will make diligent efforts to recruit a new physician(s) to the Group as quickly as possible. The FPRC will review the Group’s efforts every 12 months to determine if a reasonable effort has been made. The FPRC’s determination will take into account the general conditions for recruitment of Physicians within the region and the province as a whole.
The FPRC will not terminate a Group if the Group is making reasonable efforts to recruit the minimum number of Physicians. The FPRC will support the process by promoting the opportunities of the Blended Capitation Model to other physicians and identifying opportunities for Group mergers. The final decision on the physicians who will be part of a Blended Capitation Group – whether through recruitment or a merger with another Group – will be that of the Group Physicians.
During the period of time in which the Group continues to practice with fewer than 3 Physicians, the Group, in consultation with the FPRC, is to continue to provide services to all attached patients of the remaining Physicians as per Schedule R of the MOA; consistent with the foregoing, the FPRC will consider, at the request of the Group, a proportionate reduction in the after-hours service of the Group for this time and any extension of time as approved by the FPRC, but in any event, the remaining Physicians are to provide a minimum of 3 hours of after-hours clinics per week.
In the event a termination of a Group occurs, the Physicians will transition back to Fee for Service (FFS) in accordance with Schedule R.
The FPRC may update its rules and processes regarding transitions in Group composition from time to time.
See more about group composition in the BCM Policy Guide.
No. Members can apply to enroll in the Blended Capitation Program prior to making arrangements with a group. FPRP provides matching support to physicians seeking other group members.
Family physicians who are interested in participating in the Blended Capitation program must submit an expression of interest. To submit your expression of interest, please click here.
Continuing with multiple EMR instances in a BCG will introduce additional considerations that will require some decision-making in consultation with eDOCsNL. Moving all members of the BCG to a single EMR instance will facilitate information sharing, patient care coverage and appointment booking across physicians and practice locations in the BCG. However, combining instances will introduce a delay to onboarding to BCM in order to migrate patient data to a single instance. Please reference this graphic outlining the pros and cons of combing two or more EMR instances as you consider your best option.
eDOCSNL will perform an analysis to better understand how this scenario can work, whether there would be significant implications to consider and/or new workflows to be developed.
From a Schedule R perspective, there is nothing preventing a single location from having two BCGs. However, where two ‘co-located’ BCGs exist in the same facility, EACH BCG is responsible to ensure full adherence with Schedule R.
(For example, if a physician in BCG “A” sees a patient rostered to a physician in BCG “B”, that will be equivalent to the physician in BCG “A” seeing a non-rostered patient, with any in-basket codes billed and paid at the 100% MCP rate and part of the $56K cap for BCG A. As well, the visit can be flagged for the physicians in BCG “B” as an out of group visit, as the other members of BCG “B” should be covering for the absent physician under the model. It is also important to note that the after-hours coverage obligations under Schedule R would still be expected for each BCG in the facility, independently of the other BCG.)
Incentives, Grants, and Stipends
Grants and stipends will be released following FPRP’s receipt of the signed Letter Agreement from each physician within a blended capitation group. We are aiming for a 30 day process time.
Grants and stipends will be authorized for payment once all physicians within a BCG submit their signed letter agreements and appendices.
On the acceptance date of a newly-established Group, each member of the Group will be entitled to receive:
1. A $11, 250 Transition Grant from Government; and
2. A Start-Up Grant of $10,000 from the FPRC.
On the acceptance date of an individual physician who is joining an established Group, the physician will be entitled to receive from the Government a transition grant of $11,250. The $10,000 Start-Up Grant is not available to physicians joining an established Group. An established group is defined as a Blended Capitation Group that has been billing under BCM for 18 months or longer.
Each physician on their acceptance date will be entitled to receive from the FPRP an annual quality of care stipend of $7,500 in recognition of the physician’s participation in FPRP or practice-initiated quality programs, practice improvement and related professional development. Entitlement to the payment of this stipend will at all times be subject to the application of FPRP guidelines with respect to the professional development initiatives that will be considered as acceptable for purposes of the stipend. Please see Section 14 of the BCM Policy Guide for a list of qualifying activities. Grants and stipends will be pro-rated in the event of a Physician’s departure from the Model, as follows:
• One-Time Start-Up Grant ($10,000) – pro-rated
• Annual Quality of Care Stipend ($7,500) – pro-rated
• Transition Incentive ($11,250) – not pro-rated
• EMR Transition Grant ($30,000) – not pro-rated
Please see the Discontinuance Policy (Section 20) in the BCM Policy Guide, for details concerning the calculation and repayment of pro-rated grant and stipend funds.
Procedures Bonus
Each physician will be entitled to receive an annual procedures bonus as follows:
1. A Physician will be entitled to the bonus who bills $1,200 of in-basket Procedures fee codes (as set out in Appendix B to Schedule R of the MOA) in a calendar year, with the $1,200 measured according to 100% of MCP Medical Payment Schedule;
2. Bonus payment of $2,500;
3. Procedures bonus is payable when the above billing threshold is achieved during the year.
For the Procedures Bonus, a “calendar year” is every twelve-month period starting with the acceptance date. For physicians who join an established BCG, who have a different acceptance date from the original group, the bonus will be pro-rated in the first year according to the number of days the physicians are in the model. For example, if the group’s original acceptance date is April 1, 2024, and a physician joins the group on October 15, 2024, then the new physician would be eligible to receive a Procedures bonus on April 1, 2025, in the amount of:
$2,500/365 = $6.85 per day
Apr 1 to Oct 15 = 197 days
197 days x $6.85 = $1,349.32
Yes. However, if the new graduate is joining an established blended capitation group, i.e., a group that has been billing under the model for 18-months or longer, then the joining physician is not eligible for the Start-Up Grant.
FPRP will provide documentation related to participation in the annual Quality of Care Stipend activities by request. Physicians may contact the Blended Capitation Program at bcp@nlma.nl.ca to request a letter documenting the activities they completed to qualify for the Annual Quality of Care Stipend, as listed in Appendix A of the FPRC Policy Guide on the Blended Capitation Model.
Please note that many activities that qualify for the Annual Quality of Care Stipend, including attendance at a MyQ Blended Capitation Physician Network Call, are not associated with CPD credits. Physicians who complete CPD accredited activities should receive a certificate as part of their participation, or should request one, from the host organization.
The Blended Capitation program is happy to provide this letter to physicians to use at their discretion where they feel it will be useful.
Learners
If a learner sees one of your rostered patients on your behalf, the service will be billed at 100% fee for service (FFS).
These billings by learners will not affect the FFS cap, which is only applicable to in-basket services provided to non-rostered patients.
For the purposes of billing under the BCM, a learner is any medical student. This includes first year placement students. It does not include nurse practitioners or Practice Ready Assessment candidates.
Blended Cap Physicians should select the learner option in two scenarios:
i. when the learner assesses the patient independently (with the mentoring physician available as needed, i.e., psychiatry) or,
ii. when the learner and mentoring physician are both present in the appointment.
Note: If the mentoring physician assesses the patient independently (without the learner present), the physician cannot bill 100% FFS for a learner.
BCM physicians should only select the learner option provided that the Preamble criteria in Section 5.6 of the MCP Payment Schedule are met. A BCM physician cannot bill 100% FFS (for in-basket fee codes) without the presence of a learner in accordance with the Section 5.6 of the MCP Preamble.
Leave
Please refer to Schedule R Section 3.5 for service expectations of physicians participating in the Blended Capitation Model.
Capitation payments are paid biweekly with the expectation that care is being provided to rostered patients. In the case of physician leave (e.g., vacation, professional development, medical, and parental leave), patient care should be covered by a locum or another member of the Blended Capitation Group (BCG). Blended capitation physicians taking parental leave are eligible for the NLMA Parental Leave Allowance.
Physicians taking leaves longer than 30 consecutive days and who have not arranged for another provider within their group or a locum to cover their patients’ care will have their blended capitation payments paused during the period they are absent, from day 31 of leave until they return. Physicians are to notify FPRP in writing in advance of the dates of the leave period by submitting an Extended Leave Notification Form.
Physicians are encouraged to develop a group governance agreement to outline, among other things, how leave will be managed by the group including whether locums or other group members will be engaged to cover patient care, an understanding of what patient care is to be covered, and how capitation and FFS payments for that care will be allocated.
The program acknowledges that there may be occasions when physicians are unable to arrange care coverage for their patients including instances of unplanned leave. In such cases, the physicians should notify FPRP as soon as practicable to discuss their circumstances and to minimize payment impacts. In these instances, please email the Blended Capitation Program Manager, Melissa Sullivan, at msullivan@nlma.nl.ca.
Your BCG is required to provide a minimum of 3 hours of after-hours availability per week (see Schedule R, Section 3.5 c). If one member of the group is on vacation or leave then, per the model, the other blended capitation group members are required to cover.
The Capitation Payments remunerate the physician annually for the continuous care of their patient panel. When the physician is away from the group, a locum can be hired to provide full service unless the other members in the group agree, and are able, to provide full coverage for the away physician (including after-hours requirements).
Yes – this would be considered standard practice under BCM. But note that there may be implications concerning the NLMA Parental Leave Allowance. If full service/coverage continues to be provided by another member of your BCG, then your capitation payments will continue. However, this will likely impact the eligibility and amounts for NLMA Parental Leave as there is a limit of $1,900 per week from FFS billings and capitation payments while receiving the parental leave allowance (earnings above $1900 are reduced dollar for dollar to the weekly maximum allowance amount of $1,750), less any actual and reasonable locum costs borne by the physician. Please visit the NLMA Physician Parental Leave Allowance Program webpage for more information.
If full service/coverage continues to be provided (e.g., by a locum or another member of the BCG), then capitation payments can continue and no action is required to ensure MCP continues issuing these payments. However, this will likely impact the eligibility and amounts for NLMA Parental Leave Allowance as there is a limit of $1,900 per week from FFS billings and capitation payments while receiving the parental leave allowance (earnings above $1900 are reduced dollar for dollar to the weekly maximum allowance amount of $1,500), less any actual and reasonable locum costs borne by the physician.
If the physician is taking a leave longer than 30 days and patient care is not fully covered, then the physician is required to submit an Extended Leave Notification Form and their capitation payments will be paused as of day 31 of leave until the end of the leave period.
As per policy, in all cases, to be eligible for the Guaranteed Income Floor under BCM, full service must be provided to the patient roster by the physician, a locum, another physician in the same BCG or a combination of all of the preceding. An income floor top up would need to consider all income earned within the applicable six-month period, without locum deductions. This would include capitation payments and fee-for-service billings for out-of-basket services and for non–rostered patients. Excluded from consideration are any grants, stipends, allowances, and bonuses/incentives for which the physician is eligible under the blended capitation model.
For blended capitation physicians taking parental leave in their first two years of the program while there is a guaranteed income floor:
After the parental leave period has expired, and any applicable top-up payments are known, the NLMA will do a retroactive calculation of the physician’s earnings (as part of its typical audit procedures in relation to the parental leave allowance). Earnings will include any top-up payments divided by 26 weeks and added to any other applicable weekly income. As with fee-for-service physicians, blended capitation physicians can earn $1,900 per week, without affecting their parental leave allowance amount, whereas earnings above $1,900 are reduced dollar for dollar to the weekly maximum allowance amount of $1,750. The Parental Leave program will recover any benefit if it is later determined the physician’s parental leave payments exceeded the amount they were eligible to receive.
Please note that the portion of actual and reasonable locum costs paid by the blended capitation physician (i.e., the host physician), will be deducted from the combined FFS, and capitation payments of the blended capitation physician on a weekly basis – for purposes of the parental leave benefit only. For example, if a physician’s earnings minus locum costs totaled $2,500 per week, they would need to pay back any parental leave allowance received in excess of $1,150 per week (i.e. in the case of a physician who had received the maximum allowance of $1,750 per week: $1,900 maximum earnings per week minus $2500 actual earnings per week= negative $600; $1,750- $600= $1,150 maximal benefit per week). Please note that the preceding is a simplified example, in actuality, the maximal benefit would vary week to week based on actual earnings in that week.
Please visit the NLMA Physician Parental Leave Allowance Program webpage for more information.
No. When another physician in the BCG covers for a physician on leave and sees their rostered patients – they bill at 25%. The cap applies to patients not rostered to any physician in the BCG.
If a locum or another member of the BCG is covering patient care to ensure continuation of capitation payments, then the after-hours requirements must continue to be met. For greater clarity, if another member of the BCG is covering patient care for a physician on leave, they would be required to complete both their own and the physician’s (the one taking leave) after-hours requirements.
Locums
Locums will be paid by the blended capitation group. Capitation revenue will come to the group regularly over 26 pay periods, and this revenue is the main source of funding to pay locums when they are replacing a physician. The locum’s services will also be billed to MCP, and this serves as an additional source of funding to pay the locum. If a group chooses not to use a locum during a physician’s leave, the capitation funding will remain within the practice.
Locum arrangements may vary based on terms decided upon by the host physician and locum.
No recommendation has been developed on a locum rate.
Locum physicians will submit all billings for services rendered through the locum physician’s billing number, with the payment assigned to the blended capitation physician or blended capitation group. This will generate the FFS payment for in-basket services delivered to attached patients, as well as the FFS payment for out-of-basket services delivered to all patients and in-basket services delivered to non-attached patients.
The typical payment agreement often includes an hourly rate paid to the locum, and FFS could be kept by the host physician or paid to the locum. There are different ways those two elements can be balanced to produce a fair and appropriate arrangement. A sample contract template for locums will be developed by FPRP.
If a group chooses not to use a locum during a physician’s leave, the capitation funding will remain within the practice.
See also the BCM Policy Guide, Section 8, Locums.
Yes, FPRP now offers additional follow-up appointments with a consultant (Barbara Molgaard Blake), during which she can work with individual physicians to prepare a cash flow analysis for your practice, as well as map out potential locum payment scenarios. Click this LINK to schedule a meeting.
There is no maximum amount of time per se. However, per Schedule R, Section 3.5. d) states, “where reasonably possible, services will be provided by the physicians in a Group rather than by locums or subcontractors.”
The Capitation Rate accounts for the cost of a physician hiring a locum for two weeks of practice coverage annually. Physician leave and locum coverage is to be managed by each BCG, and locum payment is to be paid by the physician for whom the locum is providing coverage.
Patients with appointments while a locum is covering care may still be enrolled and rostered with the Blended Capitation physician in the same fashion as if the Blended Capitation physician is present and providing care.
There is no need to apply for a new Blended Capitation Locum Payee Number. When a new physician is accepted into the Blended Capitation Program a new blended capitation locum payee number is automatically generated for them and emailed to them by Provider Registration.
Each blended capitation physician gets their own individual blended capitation locum payee number to be used individually; there is no option for a single locum payee number to be issued to a blended capitation group.
The FPRP launched an advisory service to support physicians who wish to map out potential locum payment scenarios for your practice. While rates may be part of this discussion, the BCM rollout will not include a set provincial locum rate.
Please visit the booking website to look at available appointment times and book a meeting.
The FPRP has also developed a Locum Agreement Template as a tool to support Blended Capitation Groups to plan for locum coverage.
All physicians will bill 100% FFS for non-rostered patients. After a patient is rostered, the billing system will automatically convert the fee to the appropriate amount for in-basket (25%) or out-of-basket (100%) services, regardless if the primary physician or locum is providing the service. The locum will be paid by the Blended Capitation physician who is being covered by that locum.
Please also see Q 10 under Rostering: Should we wait until our entire panel is enrolled before we roster them in the billing system?
Both payments will come in a single payment. The two separate amounts will be delineated on the Remittance Statement.
Per section 3.10 of Schedule R, Blended Capitation physicians will hire and pay locums as needed and according to the arrangement agreed upon by the host and locum physicians. A Locum Agreement Template is available as a resource to support host and locum physicians in these discussions.
Locum physicians will submit all billings for services rendered through the locum physician’s billing number, with the payment assigned to the host blended capitation physician(s).
To ensure compatibility between the provincial Electronic Medical Record and the MCP system, new (non-provider number) payee numbers are being issued for locum usage in Blended Capitation-applicable situations. Provider Registration at HCS Medical Services is issuing these unique locum payee numbers to Blended Capitation practice physicians approximately a week prior to their Blended Capitation start date. Blended Capitation practice physicians will receive a single unique locum payee number that is to be used by all locums who cover their patient care going forward, while the physician is practicing under the Model.
When a locum submits a bill they must enter both their own provider number as well as the host physician’s locum payee number.
If you have commenced Blended Capitation and have not received a unique locum billing number or if you would like a locum payee number more than one week in advance of your start date, please contact ProviderRegistration@gov.nl.ca.
The same policies for fee-for-service locum activity and assignment of payment apply to this arrangement.
Two steps/forms, must be completed:
- The incoming locum physician’s provider profile must be open for fee-for-service billing, by completing the Locum Declaration Form
- The new payee number must be authorized as a payment option for the locum’s billing, by completing the Assignment of Payment Form
For more information, please review the following:
Procedure for Having Locum Physicians at a Blended Capitation Practice
Compendium: Locuming under blended capitation
The model accounts for the cost of a physician hiring a locum for two weeks of practice coverage annually. When the base capitation rate for providing care to a patient for a year was calculated, it was calculated based on average historical family physician FFS billings. On top of that number, the value of two additional weeks was added to the annual capitation rate to support a physician paying a locum to offset some of the costs of practice coverage. Compared to FFS, this represents new compensation. This boost to the capitation rate wasn’t intended to fully cover the cost of locum coverage, which will be variable dependent on the amount of time a blended cap physician takes away from practice and other factors, but to be a support. A physician can absolutely choose to hire a locum for more than two weeks and still feel comfortable that they are doing better financially than billing straight FFS.
Income Floor and Top-up Payments
Commencing on the acceptance date into the Model (the date when signed letter agreements and initialed appendices for each physician in a group are received by FPRP), each member of the Group will for a period of two years be entitled to receive a guaranteed minimum level of compensation provided to physicians participating in the Model in accordance with Article 3.12 of Schedule R of the MOA (the “Income Floor”). Payment will follow the MCP billing schedule (see the BCM Policy Guide for details).
Per the BCM Policy Guide, if in any one or more of the four six-month periods commencing on and following the acceptance date, a physician’s billings under the Model, including billings for out-of-basket services and for non-rostered patients are less than the Income Floor for each six-month period, the physician will be entitled to receive from the Government a top-up payment equal to the amount by which the Income Floor amount exceeds the Model income. Given MCP Billing rules, physicians will be topped up 90 days after the first six-month period following acceptance, then every 6 months thereafter. Once eligibility is determined, the top-up payment will be issued, as an adjustment from the Department, the next available pay period in accordance with pre-established processing cut-off dates. If there is a delay for technical reasons, the payment will be issued on the following payment date.
Example:
If a group is accepted into the Model on November 1, 2023, the physicians would continue billing FFS until they are onboarded to the BCM billing system. Regardless of when they start billing under the BCM, the physicians would be eligible for their first top-up payment as of August 1, 2024 (allowing for assessment of the six-month billing period plus the 90- day window per MCP billing rules). Physicians would be eligible for the second top-up payment at the end of the next 6-month billing period (if their remuneration remains below the income floor) on February 1, 2025, which would already include the 90-day window. After the first payment, payments would occur every 6 months.
Please Note: The determination of eligibility is a manual process and is subject to the availability of information from the MCP System, which depends upon cheque run dates which may not exactly coincide with your acceptance date. As such, it will be several weeks after the 90- day window has closed before top-up payments can be issued. The department has assigned a resource and is committed to ensure these payments are as timely as possible.
What is the formula for the calculation of the first top-up payment?
The top-up payment formula is as follows:
- Year 1 Income Floor Amount, divided by 2 (for six months).
- Subtract the physician’s total income within the BCM model, inclusive of FFS billings for out-of-basket services and for non-rostered patients, during the six-month period following the acceptance date.
If the physician’s income is less than the income floor amount, the physician is eligible for the difference in the form of a top-up payment. If the income exceeds the income floor amount, the physician is not eligible for a top-up payment.
Example 1:
- Doctor A’s Year 1 income floor, including the 10.9% adjustment, is $100,000.
- Their BCM income, including FFS billings for out-of-basket services and for non-rostered patients, is $45,000 during the six months following the acceptance date.
- Doctor A will be eligible for a $5,000 top-up payment.
| Income Floor Accepted w/+10.9% for Yr1: | |
| Income Floor Accepted w/ +10.9% for Year 1 | $ 100,000 |
| Half-year income floor accepted | $ 50,000 |
| Half-year income as defined above | $ 45,000 |
| Top-up payment | $ 5,000 |
Example 2:
- Doctor B’s Year 1 income floor, including the 10.9% adjustment, is $100,000.
- Their BCM income, including FFS billings for out-of-basket services and for non-rostered patients, is $55,000 during the six months following the acceptance date.
- Doctor A will not be eligible for a top-up payment.
| Income Floor Accepted w/+10.9% for Yr1: | |
| Income Floor Accepted w/ +10.9% for Year 1 | $ 100,000 |
| Half-year income floor accepted | $ 50,000 |
| Half-year income as defined above | $ 55,000 |
| Top-up payment | $ 0 |
This is a term of Schedule R and Article 10 (1) of the Medical Care and Hospital Insurance Act which stipulates that “A participating practitioner shall submit an account for an insured service no later than 90 days after the practitioner provides the insured service” (i.e. physicians must submit billings to MCP within 90 days of the date of service).
Both payments will come in a single payment from MCP. The two separate amounts will be delineated on the Remittance Statement.
The Remittance Statement will only display the top-up payment amount. However, the physician will receive a separate letter explaining their eligibility or ineligibility for the top-up payment.
The start and end dates of the guaranteed income floor period are clearly outlined in Schedule R, section 3.12, and therefore cannot be modified.
The Blended Capitation Model’s requirements and parameters are dictated by Schedule R to the NLMA’s Memorandum of Agreement (MOA). Schedule R was a mediated agreement between the NLMA and the Department of Health and Community Services (DHCS) that governs the development and implementation of the BCM. As part of that mediated agreement, Schedule R must be followed as written and cannot be changed without further formal contract negotiation.
We take this feedback from physicians and provide it to NLMA and DHCS to inform their discussions when the opportunity to renegotiate the terms of Schedule R arises in the future.
The Income Floor is established by Schedule R of the Memorandum of Agreement. Physicians who choose to enroll in the new payment model will receive a guaranteed income floor in the first two years to facilitate the transition. The Income Floor is calculated by averaging two recent, representative years of active practice in Newfoundland and Labrador, plus a 10.9% premium payment applied in Year One.
The Blended Capitation Income Calculation spreadsheet identifies your proposed Income Floor for Year One in the Blended Capitation Program and contains a listing of up to the last five fiscal (April 1 to March 31) years of your bi-weekly FFS billings. This data is provided by MCP for the purpose of calculating your Income Floor. It excludes: sessional fees, on-call fees, other compensation for services provided within a health authority or out of province patient claims. It is presumed that physicians will continue to provide such services into the future, and therefore would not be part of the guarantee.
Physicians who have already completed an expression of interest and subsequently submitted their practice profile to the FPRP can expect an update on their eligibility status within a few days.
Once eligibility is confirmed, FPRP will send out an email on behalf of the FPRP to each eligible physician to confirm the income floor with applicants and the Department of Health and Community Services prior to issuing letters of agreement for enrollment in the new payment model.
The email sent by FPRP will contain a link to an Income Floor Decision Form; please use the form to indicate your response to your calculation. You may choose to accept the calculation or request a review of your Income Floor.
If you indicate on the Income Decision Form that you would like a review of your Income Floor, you will be contacted by FPRP program staff to book a session to review your request and to prepare any relevant documentation for submission for reconsideration. A session with the Blended Capitation Advisor is mandatory prior to having any review of your Income Floor completed.
Your agreement to the income floor calculation will be required prior to issuance of an agreement for enrollment in the new payment model.
The Income Floor for physicians without a two-year billing history and physicians who do not have an established patient panel, will be at Step 1 from the MOA, or for a physician transitioning from a salaried position, their current Step of the Salary Scale for family physicians. The total amount will be adjusted to the proportion of FTE of comprehensive primary care the physician commits to provide in accordance with the table below. An additional 30% will be added to this amount in recognition of overhead expenses, and an additional 10.9% payable in year one of the Income Floor period.
The amount of FTE of comprehensive primary care that will be required to qualify for payment under Article 3.12 b) of Schedule R will be determined according to the number of three-hour community medicine blocks provided per four-week period.
Please click the image below for income floor calculations.
Income floors aren’t recalculated during the income floor period.
The income floor is not recalculated during the two-year income floor period, so any changes to your contract arising from negotiations will not affect your income floor.
Per Schedule R, section 3.12, the income floor for practicing physicians will be calculated by averaging the physician’s billings from two recent, representative years of active practice in Newfoundland and Labrador prior to application to the Program, excluding periods of time when the physician was away from their practice, such as time on parental leave, plus an additional 10.9% payable in year one of the Income Floor period. New graduates who do not have at least two years of billing history in NL will have their income floor set at Step 1 of the salary scale for Family Physicians (per the MOA), adjusted for FTE, plus an additional 30% in recognition of overhead expenses, and an additional 10.9% payable in year one of the Income Floor period.
In some cases, practicing physicians may have a lower income floor than a new grad, but their income floor will reflect their recent billing history and is therefore considered appropriate. Physicians may set up a meeting with FPRP Advisor, Barbara Molgaard Blake, to review their guaranteed income floor data and proposal. Please visit the booking website to look at available appointment times and make a booking.
After a BCG is accepted into the program, a Practice Facilitator will schedule a meeting to walk the Group through the enrolment and rostering processes, and eDOCSNL will contact the BCG with a few possible onboarding dates. BCGs are asked to onboard within three months of their acceptance date.
Once the BCG has met with the Practice Facilitator, it can start enrolling patients – as many as possible at a rate that makes sense for their practice. Ideally, physicians will enroll most of their patients before onboarding so they can “batch roster” them (and initiate capitation payments for those patients) in the first few days after go-live.
Depending on how quickly a BCG is able to meet with the Practice Facilitator and enroll its patients, and on how quickly it can schedule its onboarding date with eDCOCSNL, it can begin billing under the model within a few weeks of its acceptance date.
Per the FPRC Policy Guide on the BCM, physicians will be assessed for their first top-up payment 6 months plus 90 days after their acceptance date (i.e., not as part of the biweekly capitation payment). So, many physicians currently participating in the BCM may be awaiting their first income floor top-up payment and, for the time being, receiving a lower income than they received under FFS.
Another reason a physician may be earning less than they expected is that their panel may not have been fully reviewed and validated when they met with the FPRP Advisor, Barbara Molgaard Blake, to project what their income would be under BCM. Now that they are billing under the BCM, their actual patient roster may look different in terms of the number of patients and patient profile.
It is important to note that every physician’s roster is different in its demographic make-up, so capitation payments are not comparable across physicians even if they have the same number of rostered patients. The base capitation rate is modified based on the age (by 5-year age groups) and gender of rostered patients, with a younger patient profile typically resulting in a lower capitation payment than an older patient profile. And, even within this, there can be a great deal of variation depending on patient age and gender.
If physicians have not signed their letter agreement, this is reasonable. However, unless their practice pattern has changed in a material way this may be an unnecessary step.
Yes. If you provide care to patients in LTC you will bill 100% FFS for out-of-basket services to a non-rostered patient, and that would be included in the top-up calculation.
Based on section 3.10 in Schedule R, locum physicians will bill for services rendered through the host physician’s blended capitation payee number. Thus, the payments from these billings will be assigned to the blended capitation physician. So, even though the locum is performing the services, the income generated from these billings goes to the host physician and is included with the income of the host physician, in the calculation to determine whether or not the physician is eligible to receive the top-up payment from the income guarantee program.
While you are still building your roster, if you have a locum covering patient care they will bill 100% FFS for non-rostered patients. After a patient is rostered, the billing system will automatically convert the fee to the appropriate amount for in-basket (25%) or out-of-basket (100%) services, regardless if the primary physician or locum is providing the service. The locum will be paid by the Blended Capitation physician who is being covered by that locum. All MCP payments to physicians will come in a single payment, but the separate amounts – payments billed under the physicians billing number and payments billed under the physicians payee number that the locum uses – will be delineated in the pay stub.
We encourage physicians and locums to develop a locum agreement to various elements of their arrangement, including how the physician will pay the locum. A Locum Agreement Template is available as a resource to support these conversations.
Capitation Payments
Under blended capitation, each physician will receive from MCP:
- a base capitation payment for each attached patient, adjusted for each patient by the complexity modifier table attached to Schedule R;
- FFS payments at 25% of the rate in the MCP Payment Schedule for in-basket services provided to attached patients; and
- FFS payments at 100% of the rate in the MCP Payment Schedule for all other services, including services provided to patients not on the Roster of the Group.
On September 2, 2025, a new MOA was signed between the Government of Newfoundland and Labrador and the Newfoundland and Labrador Medical Association. Schedule R section 3.8 contains updated base capitation rates, effective October 1, 2023, October 1, 2024, October 1, 2025, and October 1, 2026. The capitation rate will be adjusted for each Attached patient according to the table in Schedule R, Appendix A.
Following the end of a physician’s two-year Income Floor period, the annual FFS billings of a physician for in-basket services provided to patients who are not attached patients is capped. Please refer to section 3.9 of Schedule R for the FFS limit per physician for in-basket services provided to non-Attached Patients.
For greater certainty, there is no limit to FFS billings of a physician for out-of-basket “services” to rostered and non-rostered patients.
Please refer to section 3.7 of Schedule R for a full description of the payment blend.
- Up until a patient is rostered in the billing system (eDOCSNL will provide related training during your BCG’s onboarding process to the billing system), you and/or your office staff would submit billing as per the regular process (FFS – 100% MCP billing).
- Once a patient is rostered, and a billing submission is made, go-forward payments payment will consist of a:
- Capitation payment, which is broken down and paid bi-weekly (by patient- the base capitation rate times Complexity Modifier divided by 26), and
- A fee-for-service component, which is 25% of the MCP billing for that office visit for in-basket codes as calculated by the billing system. (Out-of-basket codes will continue to be calculated at 100% by the billing system.)
- Your patient roster continues to build as each patient is attached as an ongoing process, and the capitation payment will be adjusted as patients are rostered and de-rostered in the system.
Over time, as a physician rosters more and more patients, the ratio of capitation payments to FFS payments will increase. And, the two-year income floor period provides the support of a minimum guaranteed income during this transitional period.
Please also refer to Question #10 in this section relating to cash flow, and Question #1 under Rostering for more information about patient enrollment and rostering.
If you notice an unexpected change in your biweekly capitation payment, we first advise you to consider if there was a statutory holiday(s) during that time.
Biweekly capitation payments are based on the number of days available for processing, as such if there is a holiday during the pay period that results in a delayed MCP Processing for cutoff dates, then the biweekly capitation payment for that and the following pay period will be based on the number of days available for processing. In order for the system to generate payments, an advance cut-off date is established for processing all payments as of the specific date, and some of these have to be input manually. Capitation payments, for example, would require manual inputting if a physician has no other FFS payments going out that pay period. These cut-off dates (‘cheque run dates’) apply to all payments, not just blended capitation.
Pay periods with fewer days available for consideration will have an adjacent pay period that accounts for the day(s) that were outside the view of the prior processing period. In a pay period with multiple holidays (e.g., late December), the variance may be greater. This is a result of capitation payments being calculated daily with multiple potential change factors (e.g. a patient rostering or de-rostering event, patient birthday changing the age modifier, etc.) affecting each physician’s capitation payment for any given day.
- Pay periods in 2025 that will contain fewer than 14 days of capitation payments: 25- 02, 25-09, 25-11, 25-14, 25-17, and 25-21.
- Pay periods in 2025 that will contain more than 14 days of capitation payments: 25- 01, 25-08, 25-10, 25-13, 25-16, and 25-22.
Please see this MCP Newsletter for 2025 dates and more information.
If there was no holiday or change in your roster composition to account for the discrepancy, then please contact:
Roberto Filho
Medical Services Division
Department of Health and Community Services
E-mail: RobertoFilho@gov.nl.ca
Two tools are now available to Blended Capitation physicians to help them estimate their biweekly earnings.
- An eDOCSNL tip sheet that explains how to:
- run reports to count rostered patients and estimate capitation payments; and
- obtain a detailed remittance report for fee-for-service claim payments
- A BCM Bi-Weekly Estimated Payment Calculator is an interactive tool developed by the FPRP’s Blended Capitation Program to assist physicians in estimating their bi-weekly blended capitation payments based on the characteristics of their patient roster. If you use this calculator, you acknowledge that the returned results are estimates and results may vary from actual payments calculated in accordance with Schedule R. The calculator uses roster data and physicians are encouraged to review and validate their list of attached patients prior to using the tool for best results.
If you require assistance with using the BCM bi-weekly estimated payment calculator, please book an appointment with Barbara Molgaard Blake, Blended Capitation Advisory Consultant, on the booking website.
Yes, the FPRP launched an advisory service to support physicians who wish to explore what moving to the Blended Capitation Model means for their individual practices.
Services consist of a consultant (Barbara Molgaard Blake) with whom you can book an initial meeting to explore how you can use your EMR data to define your panel of patients, predict your future income and answer any questions you may have on the Model. This information can help inform your decision on whether to move to Blended Capitation.
FPRP also offers additional follow-up appointments with Barbara, during which she can work with individual physicians to prepare a cash flow analysis for your practice, as well as map out potential locum payment scenarios. It is recommended that the BCM 60-min meeting (follow-up) session is selected if looking for assistance with cash flow analysis.
Please visit the booking website to look at available appointment times and make a booking.
The Blended Capitation rate is not based on the number of visits per year. Rather, the rate is based on 80% of what a typical physician earns in a year + two weeks locum coverage + a 21% increase (and then the complexity modifier further adjusts the rate based on age and sex of rostered patients).
A new Blended Capitation billing system will extract roster numbers from each physician’s EMR. This data will be collected every 24-48 hours and the biweekly capitation payment will be updated accordingly.
This will occur as part of regular negotiation cycles between government and the NLMA (i.e. the MOA negotiations). Note the current modifier was recently developed based upon NL data and is a NL specific solution.
The basket of services is listed in Schedule R – Appendix B.
The capitation and top-up payment processes and timelines have been reviewed by the NLMA and the Department of Health and Community Services and both partners are confident physicians should not experience significant cash flow challenges. Physicians can continue billing 100% FFS for any patients who are not rostered. Physicians can bill 100% FFS for any healthcare provided until the patient is rostered.
To ensure you receive 100% for the patient visit, create and submit the bill same day as the visit. Do not submit the rostered bill at the time of the visit as it will reduce the bill to 25% if submitted as part of the visit. The Rostered bill should be submitted on a different day after the visit to ensure there in no impact on the previous bills submitted. Once the patient has been rostered within the EMR then the physician will start receiving 1/26 payments of the cap fee every 2 weeks. Then when the patient comes in again they will bill 25% FFS for that visit.
You will still receive capitation payments for rostered patients that you see infrequently, regardless of how many appointments they have. It is important to review your roster to ensure these patients have not moved or are receiving care from a different physician, per Section 3.4 of Schedule R.
Yes. If a rostered patient travels out of province, for any reason, for any duration, their BCM physician will continue to receive capitation payments.
Per FAQ question 2 under Rostering and section 7 of the BCM Policy Guide, a patient with an expired MCP card will be automatically de-rostered from the BC billing system and they will not be eligible for billing under BCM or FFS. Capitation payments for that patient will stop for the period their card is expired. No retroactive capitation payments will be issued for the expiry period. Once the patient’s MCP card is renewed, they will have to be re-rostered to the billing system by submitting a rostering fee code in the EMR billing window, as was done for initial rostering.
Physicians may determine which of their patients have expired MCP cards in two ways:
- When a patient is automatically de-rostered by MCP due to an expired MCP card, physicians will receive a billing message in Med Access indicating a patient has been de-rostered and why. Your EMR Advisor can show you where to find these messages in your Ministry Dashboard.
- The Blended Capitation Dashboard in your EMR (turned on when groups are onboarded) displays patients you attempted to roster who have expired MCP cards. This dashboard will be demonstrated to BCG physicians during your onboarding process and your EMR Advisor can offer assistance as needed.
To avoid interruptions in capitation payments and limit payment issues associated with expired MCP cards, Blended Capitation Groups are encouraged to develop a workflow with staff to:
- call patients identified as having expired MCP cards to remind or assist them with MCP renewal; and
- check each patient’s MCP card when booking appointments and at check-in to ensure they are valid.
Yes, patients will be automatically de-rostered from the Blended Capitation billing system and capitation payments for them will stop if they: roster with another physician, move out of province, are admitted to long-term care, have an expired MCP card, or die. MCP will send physicians an EMR message indicating that a patient has been de-rostered and the reason why.
Per the Service Expectations (Section 3.5 of Schedule R) each physician will coordinate with the other physicians in the Group as required to ensure that non-emergency primary care services will be accessible to meet the health needs of the patient population served. The model is flexible enough to allow physicians in a group to divide work in the above mentioned manner, upon mutual agreement with their patients and each other, with one physician performing one type of procedure and another performing other procedures. However, there is no additional compensation under the model. Physicians in a group may choose to address these types of issues through a group governance agreement.
There is no change to the MCP claims monitoring system as a result of Blended Capitation. The MCP portion of a physician’s income will become less financially significant as physicians will receive 25% of the value of MCP billings, which will represent about 20% of their overall income. The 80% of income that is derived from capitation will be freer from administrative burden with a more straightforward billing process.
You’re correct that the long-term care codes are not in the basket of services and can therefore be billed at 100% with no cap.
Non-Rostered Patients and FFS Billing Limit ("Cap")
The updated Schedule R in the 2023-2027 MOA between the Government of Newfoundland and Labrador and the Newfoundland and Labrador Medical Association established updated FFS billing limits for in-basket services provided to non-rostered patients.
The annual limits are set at:
- October 1, 2023 $56,000
- October 1, 2024 $61,370
- October 1, 2025 $63,549
- October 1, 2026 $65,773
There is no Limit for FFS billings for the provision of “out of basket” services for rostered and non-rostered patients.
If a blended capitation physician is seeing the patient of another physician in their blended capitation group, the service they provide will be billed at 25%. The model is flexible enough to allow physicians in a group to see each other’s patients, upon mutual agreement with their patients and each other. However, there is no additional compensation under the model. Physicians in a group may choose to address these types of issues through a group governance agreement. A Group Governance Agreement Template and Group Governance Checklist are available as resources to assist BCGs with these discussions. See section 4.5.1 in the Group Governance Agreement Template, which addresses cost sharing for patient care.
No, if you see a patient who is rostered to another physician in your BCG, you can bill 25% FFS for any in-basket care and it will not count toward the limit (“cap”). Out-of-basket services for all patients are billed at 100% FFS and do not count toward the limit (“cap”).
Any in-basket services that you bill for non-rostered patients will be counted toward the FFS billing limit (“cap”). Out-of-basket services for both rostered and non-rostered patients do not count toward the FFS billing limit (“cap”).
The model is designed around providing care to rostered patients, with the FFS billing limit (“cap”) providing flexibility to see some non-rostered patients.
Per Schedule R, Section 3.9, there is no FFS billing limit (“cap”) during a physician’s first two years in the model. After the two-year income floor period, any FFS billings for in-basket services provided to non-rostered patients will be capped at the amount set in Schedule R, section 3.9. There will be no remuneration under the BCM for billings exceeding the FFS billing limit (“cap”). Note there is no limit to FFS billings for out-of-basket services provided to rostered and non-rostered patients.
MCP will include a message to notify physicians who are approaching their FFS billing limit (“cap”) in their billing remittance statement.
No. Per Schedule R, Section 3.9, the FFS billing limit (“cap”) will be implemented following the two-year Income Floor period. This allows two years for Blended Capitation physicians to bill at 100% FFS for non-rostered patients while they merge their EMRs and roster their patients.
Performance Indicators
The appointment availability metric (i.e., same day and next day availability) will be measured at the group and individual level. However, if your BCG has worked out a system that all members agree with and if performance expectations are being met at the group level, then the program does not anticipate any issues. Your group may wish to outline the parameters and responsibilities of your same day clinic in a Group Governance Agreement to ensure everyone agrees. Resources to help you develop a Group Governance Agreement are available here.
The objective of the performance indicators process is to encourage continuous improvement and/or maintenance of accessibility and high-quality care. Therefore, there are no specific targets or goals attached to these, with the exception of after-hours access.
The approach for defining and measuring access relies on three performance indicators, listed below:
- Percentage of same-day or next-day appointments available to attached patients.
- After-hours access provided to attached patients. This indicator will be based on the after-hours service expectations, which is driven by a formula. To determine your group’s after-hours requirements, please refer to the After-Hours Expectation Calculator.
- Relational continuity, meaning the ongoing therapeutic relationship between a family physician, including their team, and an Attached patient. This indicator will measure the proportion of visits by attached patients to their family physician, and to their family physician’s Blended Capitation Group.
The monitoring and evaluation plan is in development and will be communicated to BCGs when finalized.
Practice Facilitation Services
Practice facilitators play a vital role in helping practices identify and implement processes to optimize their day-to-day operations and enhance the overall quality of care delivered. Practice facilitation support is personalized and responsive, with facilitators meeting each clinic where they are in their journey, tailoring support according to the clinic’s unique needs and priorities. By leveraging national resources and best practices, facilitators help strengthen quality improvement, collaboration, and engagement within the clinic teams. Additionally, practice facilitators ensure practices receive the information and support needed to navigate the BCM effectively by connecting them with the appropriate program resources.
To book with our Practice Facilitator, please email bcp@nlma.nl.ca.
Rostering
There are two steps to adding patients to your Blended Capitation roster:
- Patient Enrolment – The Blended Capitation Program has developed a patient enrolment form and information sheet to support the patient enrolment process. It will be available in Med Access after all physicians within your Blended Capitation Group have submitted their signed letter agreements and initialed appendices. With each patient visit, you/your office staff will discuss the enrolment form with patients as part of the check-in process, and the patient’s consent to be enrolled with their physician will be documented in the Med Access form. The enrolment process may also be completed over the phone, with consent recorded in the Med Access form.
- Patient Rostering – after your patient has consented to enroll with their physician, they can be rostered in the Blended Capitation billing system by: i. Checking the ‘Blended Capitation’ box, and ii. submitting a Blended Capitation fee code to MCP in the EMR billing window, using the new EMR Blended Capitation functionality. These features will be available to you when your group is onboarded to the BCM. This second step officially rosters the patient and generates capitation payments to the physician.
As part of your BCG onboarding process, the Blended Capitation Practice Facilitator and an EMR Practice Advisor will provide demonstrations, training and support related to patient enrolment and rostering workflows at your clinic. For more detailed information regarding the enrollment and rostering process please view the eDOCSNL Tipsheet.
For guidance related to potential cash flow issues during rostering, please view question #10 in the Capitation Payments section above.
Due to an MCP system limitation, when a patient’s MCP card expires, they will be automatically de-rostered from the Blended Capitation billing system and they will not be eligible for billing under BCM or FFS. When a patient is de-rostered from the BCM billing system, MCP will send a notification to the physician that their patient was de-rostered via an EMR message.
Once a patient’s MCP card is renewed they can be re-rostered in the BCM billing system by resubmitting the Blended Capitation fee code in the EMR billing window (as done for initial rostering).
To limit issues with expired MCPs, office staff are encouraged to check patient’s MCP cards when booking appointments and at check-in to ensure they are valid before care is provided, and if the card is close to expiry to remind them to renew online. eDOCSNL has added a reporting feature to EMR that allows users to generate reports of upcoming MCP expiries so that clinics can identify and ask patients to renew in advance. Please contact your clinic’s EMR Practice Advisor or info@edocsnl.ca for assistance.
If a patient opts not to roster, the physician can continue seeing them and bill FFS (subject to Section 3.9 of Schedule R, “3.9 FFS Billing for Non-Rostered Patients”). After the two-year Income Floor period, the FFS billing limit per physician for in-basket services provided to non-rostered patients is established in Schedule R, Section 3.9. Refer to Question #1 in the Non-Rostered Patients and FFS Billing Limit (“Cap”) section above. There is no limit for FFS billings for the provision of “out of basket” services for rostered and non-rostered patients.
The after-hours requirements relate to rostered patients, but physicians could choose to make after-hours clinics available to other patients (keeping in mind performance indicators).
While the majority of a physician’s patients will likely become rostered over time, some patients may remain outside the roster. This is ok but physicians must fulfill their commitment under Schedule R to providing comprehensive and continuous care to all of their patients: Section 3.3 (a) of Schedule R states that all family physicians will be eligible for payment through the Model, provided they “commit to provide comprehensive continuous primary healthcare services across the life span of their patients, based on patient needs and responsive to documented needs of the geographic community they serve.”
It should be noted that, per section 3.9 of Schedule R, in-basket services provided to patients who are not rostered will be subject to a FFS billing limit (“cap”) after the two-year income floor period ends.
Patient enrolment does not have to occur alongside a patient appointment. Physicians or their office staff may contact their patients by phone to initiate the enrolment conversation, review the Patient Enrolment Information Sheet, and elicit patient consent to enroll, which can be recorded in the electronic Enrolment Form in Med Access. The Patient Enrolment Information Sheet should be emailed to patients where possible. The patient Enrolment Form is located under the task category of Form (Blended Capitation Enrollment) in MedAccess. The information sheet is on page 2; you will need to click on the green arrow to access it.
To identify patients who visit the practice infrequently, EMR reports can be generated to list patients who have not been seen for more than a year and who do not have an upcoming appointment.
Workflows will be discussed during the onboarding sessions with eDOCSNL and FPRP.
Yes. Blended capitation requires a relationship between a patient and a most responsible provider. Under the Blended Capitation Model, two doctors can choose to share that care and see each other’s patients for both after-hours care and for routine medical appointments. However, patients would need to be rostered to one doctor for the purpose of payment.
You can begin enrolling patients as soon as your group is accepted into the Blended Capitation Model (BCM) but rostering (which involves entering a rostering fee code and clicking a “blended capitation” box in the EMR billing window) cannot occur until you are onboarded to the Blended Capitation billing system. You are advised to enroll as many patients as you can now.
No, you don’t need to wait until you’ve enrolled your entire panel to start rostering. Accepted Blended Capitation physicians should start enrolling patients now at whatever speed makes most sense for them given the nature of their practice. However, they are encouraged to enroll patients as soon as reasonably possible while they are waiting to be onboarded to the billing system. Then once they are onboarded to the billing system, they can roster all those enrolled patients on the first day.
Patients will be automatically de-rostered from the Blended Capitation billing system and capitation payments for them will stop upon:
- admission to a Long Term Care Facility, meaning a publicly-operated long-term care facility providing on site professional health and nursing services;
- the patient’s death;
- removal from the Roster by the physician;
- an expired MCP number (card);
- an invalid MCP card;
- federal incarceration;
- a patient has been rostered by another physician;
- or a physician’s roster limit has been reached.
MCP will send physicians an EMR message indicating that a patient has been de-rostered and the reason why. Please review the eDOCSNL Tipsheet for more information about de-rostering.
If a newborn is receiving care from the provider before they have their own MCP, they cannot be rostered under the Blended Capitation Model and are billed under their mother’s MCP. Once the baby has their own MCP they can be rostered and billed under the Model. Until the baby gets their own MCP card there is no associated capitation payment.
Per Schedule R, patient attachment must be confirmed (via the enrollment process) before they are rostered to the BC billing system.
When a date for onboarding is suggested by eDOCSNL, BCGs are required to schedule their onboarding within a reasonable timeline from that date (i.e., within 3 months). When you have confirmed your onboarding date with eDOCSNL, please make every reasonable effort to adhere to the date selected unless extenuating circumstances arise. eDOCSNL must allocate dedicated resources to support onboarding blended capitation groups which must be coordinated between supporting other blended cap groups and the many other expectations that eDOCSNL personnel are required to meet. In the event of extenuating circumstances, please communicate with the eDOCsNL team to identify an alternate date.
In preparation for onboarding, accepted blended capitation groups are encouraged to begin enrolling patients as soon as reasonably possible, at a pace that suits their practice. Then, once your blended capitation group is onboarded to the billing system, you can roster all enrolled patients on the first day.
Please note, patients must be enrolled before they can be rostered (attachment is a requirement of Schedule R).
No. Enrolment is the formal process to confirm attachment between a patient and their primary provider. Unless a patient is a child under 16 years or a dependent adult, they must agree to enrollment themselves.
Groups that have been accepted into the Blended Capitation Model may telephone patients to conduct the enrollment process or enroll patients when they come into their office for an in-person appointment. The Information sheet can be read to the patient over the phone and the patient’s confirmation of enrollment can be given verbally and recorded in the electronic Patient Enrollment Form in Med Access. Patients’ confirmation of enrollment (signatures are not required) can also be received via secure email but will have to be manually entered into the electronic Patient Enrollment Form in Med Access.
Physicians may roster patients at whatever speed makes sense given the nature of their practice, but are encouraged to roster patients as soon as reasonably possible. All patients should be rostered within 2 years from a blended capitation group’s acceptance date into the model, during which time the group’s members are eligible for the guaranteed income floor. At the end of the 2-year income floor period, non-rostered patients can be billed @ 100% FFS up to a maximum of the established FFS billing limit (“cap”) annually for in-basket services (per Schedule R, section 3.9. and Question #1 in the Non-Rostered Patients and FFS Billing Limit (“Cap”) section above). Out-of-basket services for non-rostered patients can still be billed 100% FFS (no limit).
If patients have an appointment in the near future, it may be best to see them first at their scheduled visit, submit your service fee at 100% FFS and then roster them the next day, in a separate batch than the service bill. You can utilize telephone outreach to contact and enroll patients that you see infrequently (for example, no appointment in the past two years), generate reports and roster those individuals in batches on your Go Live date to begin receiving capitation payments for those patients.
Yes. There are scenarios where a physician may learn of a patient’s death (e.g., when offering palliative care) before it is captured in the death registry and communicated to MCP. In such cases, you are advised to de-roster this patient and unclick the Blended Capitation box in the EMR billing window to ensure capitation payments for that patient stop.
Yes, please change the rostering fee code to reflect their new gender classification.
Physicians are advised to use their discretion when selecting the sex/gender (e.g., male, female, other) to submit the rostering fee code. Their selection does not have to match the sex/gender captured in the MCP system. Notwithstanding the above, a cis-male should be selected as male and a cis-female should be selected as female.
Your roster counts will be visible in your EMR Blended Capitation Dashboard that will be available to you once you’re onboarded to the program. Your EMR Advisor will demonstrate the Dashboard’s features and information as part of your onboarding process. Please bear in mind that you will be able to see what you submitted on your dashboard, but the roster count will always be most accurate in the MCP system. The count displayed in your EMR may not match MCP’s count at a given point in time due to, for example, patients being de-rostered on the MCP side due to an expired MCP, rostering with another provider, etc. See FAQ#11 under Rostering for other reasons a patient may be de-rostered by MCP.
Service Expectations
After hours expectations for rural physicians are the same as for all physicians participating in the Blended Capitation Model.
The Group must be committed to using its best efforts to provide its Roster of patients availability and timely access to excellent team-based primary care. The Group will establish, based on the primary care needs of its Roster, a schedule for the regular weekly availability of non-emergency priority care. This does not mean that every physician within the Group must work Monday through Friday, 9 am to 5 pm. Rather, it means that regular availability must be established each week in relation to Roster size, with recognition that physicians may set aside time for other medical activities, administrative activities, or have a part-time practice. See Section 8 in the BCM Policy Guide.
Physicians who work part-time (e.g. two days a week with a roster size of 400 patients) may still enroll in the Blended Capitation Model as long as they provide comprehensive longitudinal services to their roster and meet access indicators. Physicians within the group may be part time as long as there is “reasonable, regular hours each week of the year”, including the required after-hours access, which can be shared among the overall group.
The after-hours requirement does not require more hours of work per week. It only requires the group to schedule a portion of its work outside the 9am-5pm, Monday-Friday window.
There is a formula for the number of hours per week of after-hours care linked to the total number of rostered patients. For example, a group with 3,600 patients must provide a minimum of 6 hours of after-hours care each week. This obligation is divided among the doctors within the group (e.g., for three doctors it could mean 2 hours each per week, or 6 hours per doctor for one week out of three). The after hours requirement increases in proportion to the number of patients attached to the group. See Section 3.5 (c) in Schedule R.
An After-Hours Expectation Calculator has been developed by the FPRP’s Blended Capitation Program to assist physicians in estimating their after-hours expectation based on the number of patients rostered to the blended capitation group. By using this calculator, physicians agree that the returned results are estimates and results may vary from the actual after-hours expectation required under Schedule R. The calculator uses roster data and physicians are encouraged to review and validate their list of attached patients prior to using the tool for best results.
If you require assistance with using the After Hours Expectation Calculator, please book an appointment with Barbara Molgaard Blake, Blended Capitation Advisory Consultant, on the booking website.
This is a decision of the group, and will be guided by FPRC policy. Here are some examples:
In a group of three physicians serving 3,600 patients, the obligation is 6 hours per week for the whole group.
- Option 1: The physicians choose to take turns providing a Saturday clinic on rotation (one Saturday every third week for 6 hours). When a physician provides the Saturday clinic they can book one of their regularly scheduled clinic days off, to maintain a normal workload.
- Option 2: On two days a week each physician might open at 8am or close at 6pm. They can also keep the same number of total hours each day to maintain a normal workload.
- Option 3: Every week there is a Wednesday clinic from 5-8pm and a Saturday clinic from 9am to 12noon, for a total of 6 clinics every three weeks. Each of the physicians may cover two of the clinics in a three week period, and take time off during the week to maintain a normal workload.
In a group of four physicians serving 4,000 patients, the obligation is 6.8 hours per week for the whole group. If three physicians have panels of 1,200 patients each, and the other physician has a panel of 400 patients, the physicians can choose to divide the after-hours expectation according to their patient loads. For example, once a week each of the three physicians with larger panels could stay open two extra hours, and the physician with the smaller panel could extend by one hour. To accommodate for the later hours, they could adjust the start time of their workday.
The expectation is that doctors in a group will make their after-hours care available to all the patients attached to physicians within the group.
Yes. Any appointments outside the regular hours of Monday to Friday, 9am to 5pm, meet the after-hours requirement.
No, only NPs employed by or directly contracted by the BCG count.
The objective of the performance indicators process is to encourage continuous improvement and/or maintenance of accessibility and high-quality care. If a Group (or an individual physician within a Group) is not maintaining accessibility or quality of care, consistent with the above objective, based on the performance indicators, the FPRC will engage the Group or the physician in a process of information exchange and performance improvement. If, following these activities, improvement has not been achieved, the FPRC will have discretion to terminate the Group (or an individual physician within a Group) from the Program (per Section 3.6 d) of Schedule R).
In regards to after-hours requirements, per Schedule R, section 3.5 c), the Blended Capitation Group (BCG) is required to provide after-hours clinics to attached patients as follows: 2.2 hours per 100 patients on the total BCG roster, with a minimum of 3 after-hours per week per BCG. See the table in section 3.5. c) for details. All physicians in a group will participate in after-hours service expectations. After-hours performance will be measured at the Group and individual level. However, if a BCG has worked out a system to meet the after-hours requirement that all members agree with, and if performance expectations are being met at the group level, then the program does not anticipate any issues. BCGs may wish to outline their plans for covering after-hours requirements in a Group Governance Agreement to ensure everyone agrees. Resources to help groups develop a Group Governance Agreement are available here.
In regards to “activity in a quarter”, per Schedule R, section 3.5 e), to achieve excellent availability of and access to team-based primary care, each BCG is recommended to provide an average service level not fewer than 88 attached patient care encounters per 100 attached patients each 13-week period. Aspiring to this level of activity will allow physicians to spend more time with patients and achieve improved work-life balance. This performance indicator will be measured at the Group level and, per above, where a BCG is not meeting this recommended level of activity, the FPRC will engage the Group in a process of information exchange and performance improvement to work toward a greater number of encounters for attached patients. Unlike the after-hours requirement, the FPRP does have greater discretion when it comes to the recommended activity level, depending on the circumstances encountered when it engages with a practice in this regard. As such, the 88 encounters is not a strict requirement.
Example:
If a physician has 1,500 rostered patients, this means they are recommended to provide 101.5 visits per week (1,320 per quarter). Assuming the other BCG physicians have the same roster size, the BCG is recommended to deliver 304.6 visits per week (3,960 per quarter) for the total group roster of 4,500 patients.
Calculations: Physician
| Roster size | 1,500 |
| 1,500/100 | 15 |
| Visits per quarter (15×88 attached encounters) | 1,320 |
| Visits per week (1,320/13 weeks) | 101.5 |
Calculations: Group of three physicians
| Roster size | 4,500 |
| 4,500/100 | 45 |
| Visits per quarter (45×88 attached encounters) | 3,960 |
| Visits per week (3,960/13 weeks) | 304.6 |
| Visits per week per physician (in group of 3) | 304.6/3 = 101.5 |
This function sits with FPRC. Section 3.6 e) of Schedule R sets out FPRC’s role to develop definitions and guidelines for the performance indicators, and Section 3.6 f) to monitor them.
The after-hours requirement starts on the date the Blended Capitation Group is onboarded to the billing system.
FTE equivalency is only used to calculate the income floor for physicians without a 2-year billing history. For those physicians, the amount of FTE of comprehensive primary care that will be required to qualify for payment under this section will be determined according to the number of three-hour community medicine blocks provided per week, on average over a four-week period (i.e. 1.0 FTE = 27 hours of community-based primary care; 0.8 FTE = 21 hours of community-based care).
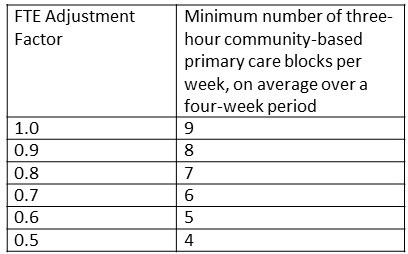
For physicians with a two-year billing history, the income floor will be established using two recent representative years per section 3.12 of Schedule R. However, if you have recently, or soon plan to, reduce the size of your community-based practice, or otherwise expect a reduction in your billing income, please indicate that you do not accept the Income Floor on the form. You will be contacted by the Blended Capitation Advisor to develop a solution customized to your circumstances.
The objective of the Performance Indicators is to encourage continuous improvement and/or maintenance of accessibility and high-quality care. Capitation payments will not be withheld due to occasional or infrequent instances of unmet service expectations.
However, if the FPRC considers that a group or a physician is not maintaining accessibility or quality of care, consistent with the set expectations, the FPRC will engage the group or the physician in a process of information exchange and performance improvement.
If following such engagement, the FPRC concludes that the necessary improvement has not been achieved, the FPRC may in its discretion terminate the group or an individual physician from participation in the Program. Please see the BCM Policy Guide.
